How a medical practice changed its approach to pain
Calderside Medical Practice in Lanarkshire has moved from treating persistent pain as a symptom that needs a drug to treating it as a long-term condition that can be managed with information and support.
Since changing their approach in 2016 they have registered around 300 patients with pain and have halved their prescribing of both opioid and gabapentinoid medicines. Patients at the practice find they need to attend GP surgeries less frequently since they have benefitted from rehabilitation through pain management consultations with access to multi-disciplinary support.
Dr Kieran Dinwoodie, one of the doctors at Calderside Medical Practice, gives his perspective on this approach.
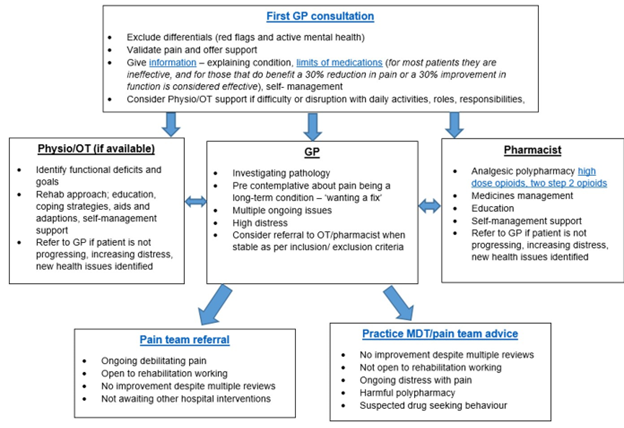
Consultation Model
My consultation model is based on building trust. This means my patients have to feel heard, validated and supported. This helps move the conversation on from ‘what’s the matter’ through to ‘what matters to you?’
First Consultation
At the first consultation there are often multiple problems and high emotions. It is not possible, or fair, for the patient (or for me!) to try and manage this in ten minutes.The goal is to build a relationship, not fix a problem. I start with the biomedical assessment to make sure there are no indications of underlying problems that need to be investigated. I also check if there are active mental health problems. The next step is to be honest and let the patient know there is no magic tablet, and that this is a long-term condition in its own right. I explain that I will work with the patient to improve their quality of life. At the end of the first consultation I tell the patient about the practice website which has lots of clear, easily-accessible resources offering information and support. We then follow up in around one month.
Follow Up
At the follow up consultation, I focus on the pain management plan and especially goals for what the patient wants for themselves. At this point we also discuss medication options. This might mean screening for neuropathic pain, and ensuring any medication is appropriate. Also, if there are associated mental health problems, I discuss appropriate medication that might be helpful.
Support
Many people need more support than their GP can offer. Having access to skilled practitioners and voluntary organisations helps improve outcomes. The key is trust and for people to feel supported. Our occupational therapist helps our patients improve their daily functioning and our pharmacist helps with supported opioid and gabapentinoid reductions.